Dr. Hila Robbins in Los Angeles, CA – Patient Education
Pediatric Dentistry: An Integrative, Multidisciplinary Approach

As a DMD (Doctor of Medical Dentistry), specializing in pediatric dentistry, Dr. Hila Robbins in Los Angeles, CA, has years of advanced, post-doctoral academic and clinical training, extending well beyond care for children’s teeth. Dr. Robbins‘ training spans the full continuum of childhood development, from infancy, early childhood, and adolescence.
At Dr. Robbins’ office, we always consider the health and well-being of the entire patient, not just the patient’s teeth, gums, and oral cavity. This approach is sometimes referred to a biological dentistry. Comprehensive initial exams, diagnostic procedures, prescribed treatments and recommended patient follow-up take into account, if indicated by patient history or initial findings, the presence not only of common and usually correctable conditions (for example, cavities and tooth crowding), but also the existence of congenital conditions, the risk or existence of childhood diseases, functional and behavioral issues, and/or special needs.
Also trained in orofacial myofunctional therapy, Dr. Robbins can identify and treat functional factors and behaviors that may affect breathing, speech, breastfeeding, chewing, swallowing, facial development, sleep, posture, and movement. Additionally, Dr. Robbins is trained in cranial nerve assessment, neuro-sequencing and cranial-osteopathic concepts relevant to dentistry, fascial anatomy and function, and management of head and neck pain; fields which can lend important insight into patient diagnosis and treatment, often including close consultation and active collaboration with other specialists.



Dr. Robbins’ advanced training, experience in private practice, in university-based pediatric dentistry at UCLA and the world renowned Children’s Hospital of Philadelphia, and her commitment to continuing education means that our patients benefit from Dr. Robbins’ extensive range of clinical knowledge and practical skill.
Note: We provide the following information for educational purposes only, not for diagnosis or treatment, which must only be done by qualified practitioners. More detailed information can be found in the research and clinical literature and through online searches of reputable sources, such as those found on our Helpful Online Resources web page. Some of the information below draws upon material covered in New Trends in Myofunctional Therapy – Occlusion, Muscles, and Posture. Edi. Ermes s.r.l. 2020, for which Dr. Robbins was an editorial collaborator.
We list the topics below in alphabetical order.
ALF / Quantum ALF Appliance
Dr. Robbins is highly experienced in using the ALF appliance (developed/invented by Dr. Darick Nordstrom) and is a Certified ALF Provider. Based on clinical feedback from myofunctional therapists and osteopathic physicians, the ALF (Advanced Lightwire Functionals) is a wire appliance, designed to facilitate the natural development of the oral cavity and associated structures, to achieve optimal function.

The ALF (now referred to by some providers as the Quantum ALF) provides a more gentle way to expand the maxilla and mandible and align the teeth, working in harmony with the body’s natural growth patterns and physiologic rhythms. The ALF has been used to treat a range of anatomical and physiological issues, including cranial bone and soft tissue and airway development, orofacial pain), sleep issues, vision issues, myofunctional disorders, and postural alignment issues.
Breastfeeding in Infants
Dr. Robbins often collaborates with pediatricians, lactation consultants, and other early childhood specialists to help address breastfeeding issues in newborn babies and young infants. Lack of desire to breastfeed, failure to latch, difficulty swallowing, and excessive or painful irritation may indicate the presence of tongue-tie, lip-tie, or other oral anatomical or functional issues that impede optimal breastfeeding and are amenable to safe and effective treatment under the care of an appropriately experienced and equipped pediatric dentist and other specialists. This experience includes the education of moms and dads on pre-treatment expectations and preparations and the importance of post-treatment exercises to ensure successful and lasting results.
Dr. Robbins is a specially trained BabyLase provider. BabyLase is a non-surgical therapy for release of oral tissues in babies and toddlers experiencing breastfeeding difficulties due to oral tissue restrictions.
Cranial Nerve Function and Sequencing
The cranial nerves control many functions of the mouth, jaw, face, head, and neck, such as the movement of the facial muscles and the muscles of the lips, tongue, mastication (chewing), and swallowing, as well as salivation (saliva production) and the senses (taste, smell, vision, hearing). There are 12 pairs (right and left) of cranial nerves that emerge directly from the brain and brainstem, conventionally numbered I-XII. Cranial nerve X, the vagus (“vay-guss”) nerve, provides both muscle and sensory inputs to the head and organs in the chest and abdomen. Normally, all the cranial nerves work together in near-perfect sequence, coordinating the exquisitely fine-tuned head and neck functions, and especially important to dentists, the mouth! Sometimes, due to developmental issues, injury, or abnormal pathology, the cranial nerves may not function optimally; they may operate “out of sequence,” which affects the ability to integrate muscle and sensory functions.
Dr. Robbins has taken advanced training to assess cranial nerve function as part of her overall multidisciplinary and integrative approach to pediatric oral care and wellness. Some issues may be addressed through a process of neural sequencing to achieve optimal coordination of certain functions and behaviors related to dentistry. Dr. Robbins may also recommend consultation with other specialists, as in the case of injury, anatomical anomalies, or pathology that may affect the cranial nerves.
Pain Evaluation and Treatment Approaches
As a Senior Clinical Instructor in the TMJ/Craniofacial Pain Clinic of the Audiology Foundation at White Memorial Medical Center, Los Angeles, Dr. Robbins has advanced training and experience in evaluating dental, oral, facial, head and neck pain in pediatric patients. Pain can arise from various causes and may also be perceived by the patient at a site or location distant from the actual cause. This particular type of pain is known as referred pain.
The evaluation of pain calls upon a range of methods, including patient reporting, questioning, observation, and physical examination by the practitioner, usually done by direct palpation affected areas with the fingers and other exploratory procedures, such as imaging. Evaluating pain in children draws upon the pediatric specialist’s skillfulness in communication and observation, mainly because very young children or kids with special needs may not vocalize or explain their pain.
Neurologic pain is usually described as headache, sharp, burning, stabbing, pins and needles, or a sensation akin to electrical shock. Muscular pain tends to present as a dull ache and may persist. Upon palpation of the affected tissues, muscle pain may be reproduced. Muscle pain may result from postural problems, chewing problems, joint function problems, and overuse or maladaptation to repeated stress. Pain may also arise from soft tissue injury (cuts, abrasions) or secondary to infection as with an abscess, and, of course, tooth eruption or cavities.
Using an integrative approach, Dr. Robbins evaluates pediatric dental, oral, facial, head and neck pain by considering not only the immediate symptoms but also, the root causes and contributing factors, which can include habits, behaviors, or activities that place inordinate stress on muscles and joints of the head and neck. Some notable causes of dental-related and referred pain in children include teeth grinding, clenching, or bruxism. Another possible source of pain is excessive and “ergonomically challenged” use of handheld electronic devices, such as smartphones, tablets, etc., a problem not limited to children! Depending upon each child’s complaint of pain and initial findings, Dr. Robbins may suggest additional evaluation, recommend specific behavior changes, or advise a particular treatment plan. Because pain may arise from multiple causes, including health issues outside of the pediatric dentist’s typical scope of practice (as may be the case, for example, in certain kinds of neurologic pain), Dr. Robbins may also suggest a consultation with other specialists as part of a multidisciplinary approach.
Laser Dentistry in Pediatric Patients
Dental Lasers
The word “laser” is actually an acronym for “light amplification by stimulated emission of radiation.” In simple terms, a laser is a device that generates and emits a high energy beam of light of that can be used to perform work, such as the cutting of materials, including biological tissues. The FDA has cleared for use a variety of dental laser devices for diagnostic, therapeutic and cosmetic procedures. Lasers are classified according to the type of light source, which determines such characteristics as wavelength, frequency, and pulse duration, which, together, determine the laser’s specific clinical applications.

Types of Lasers Used in Dentistry
The two main types of lasers used by dentists are hard tissue and soft tissue lasers. In the mouth, hard and soft tissues absorb laser light in different ways, depending on the physical and chemical composition of the tissue. Hard tissues, such as teeth, are composed largely of crystallized calcium phosphate minerals, whereas soft tissues, such as the gums, or the flap of connective tissue beneath the tongue, consist largely of water and other biological molecules, such as hemoglobin (which carries oxygen in red blood cells).

Hard Tissue Lasers
In dentistry, a hard tissue laser is used primarily for cutting teeth, as an alternative to mechanical drilling with a burr or bit. Hard tissues lasers can cut very precisely, making them ideal for certain kinds of cavity preparations. The dentist determines which type of cutting instrument is ideal, based upon tooth anatomy, extent of decay, and other factors.
Soft Tissue Lasers
Soft tissue lasers use a wavelength of light that is readily absorbed by hemoglobin and water molecules, making this type of laser ideal for cutting soft tissues that contain blood vessels. In pediatric dentistry, soft tissue lasers may be used to “release,” or remove connective tissue that may restrict proper movement of the tongue or lips (conditions referred to as tongue-tie and lip-tie). Soft tissue lasers may be employed by the dentist as an alternative to, or in conjunction with, bladed surgical instruments (scissors, scalpel), depending on such factors as the location and thickness of tissue to be treated.

Dr. Robbins is a specially trained BabyLase™ provider. BabyLase is a type of laser-assisted therapy that encourages non-surgical “softening” of tight tissues that can help patients with nursing and other conditions and to guide patients to better function.
Movement & Posture
Consider this: Kids need to move! Physical activity, especially play, is vital to healthy growth and development in children, and pediatric dentists can play an essential role in educating parents about the importance of encouraging healthy movement and posture in children.
As part of her everyday patient interaction, Dr. Robbins helps parents to “be on the lookout” for behaviors and activities that, if not addressed or corrected, can lead to later problems because of untoward muscle strain, repetitive motion, impingement of cranial nerves, mouth breathing, and airway problems. Examples of potential “problem” behaviors and activities include overuse of handheld mobile devices (smartphones, tablets, etc.) that induces unhealthful forward head posture, lack of active, physical play, poor seated posture, and sleeping positions that constrain the airway.
Dr. Robbins is highly trained and experienced in observing and correcting problematic behaviors and habits related to unhealthful movement (or lack thereof) and improper posture. She is a certified instructor in GYROKINESIS® and GYROTONIC®, which are complementary movement methods, originally developed to help injured dancers regain strength and agility.
Don’t be surprised if Dr. Robbins gives you and your children a Prescription for Play!
Oral Myofunctional Therapy
Oral myofunctional therapy (abbreviated OMT, commonly called “myo”) is a technique to treat symptoms relating to breathing disorders, sleep apnea, TMJ (temperomandibular joint) disorder, and other ailments that often emerge in early childhood. Experts in pediatric OMT (myo for children) are professionally trained to diagnose treat conditions and “bad habits” of the lips, tongue, airway, facial muscles, and head/neck positioning (posture) that may otherwise persist into adolescence and adulthood. Dr. Robbins is a thought leader in integrating oral myofunctional therapy into a comprehensive pediatric oral care plan and development plan. She interacts with an extensive network of OMT therapists throughout California, nationally, and internationally.
Sleep-Disordered Breathing
Sleep-disordered breathing (SDB) describes a group of clinical symptoms and events caused by an abnormal increase in resistance to air passage through the upper airway during sleep. Two commonly known examples of SBD in both children and adults are snoring and obstructive sleep apnea. There are other, less commonly known types of SDB. Common symptoms of SDB include nighttime snoring, pauses of breathing during sleep, bruxism, awakening with choking, dry mouth, and daytime sleepiness. It is not unusual for SDB to be diagnosed following the identification of behaviors in affected children, such as mouth breathing while awake (breathing through the mouth with open lips, rather than through the nostrils), forward head posture, daytime sleepiness, irritability, and inability to concentrate.

The importance of detecting and treating sleep-disordered breathing during childhood cannot be understated. SBD during childhood can be a risk factor for other health problems, including chronic issues in adulthood. Fortunately, SBD can be adequately diagnosed and treated in children, using a multidisciplinary approach that may involve specialists in pediatric dentistry and medicine, sleep medicine, otolaryngology (ENTs), myofunctional therapists, cranial-osteopathic physicians, and other practitioners. Dr. Robbins favors a natural, gentle approach to achieve optimal treatment outcomes for SBD and likes to emphasize the importance of good sleep hygiene for overall health and development in children.
Tongue-tie and Lip-tie
Tongue-tie and lip-tie are two terms in common usage to describe the presence in the mouth of connective tissue (known as a frenulum, or, sometimes interchangeably, as a frenum) that restricts the normal range of movement of the tongue or lip (upper, lower or both). The presence of tongue-tie or lip-tie can cause or contribute to breastfeeding problems in infants, and, later, difficulties in chewing, drinking, swallowing, and speech.
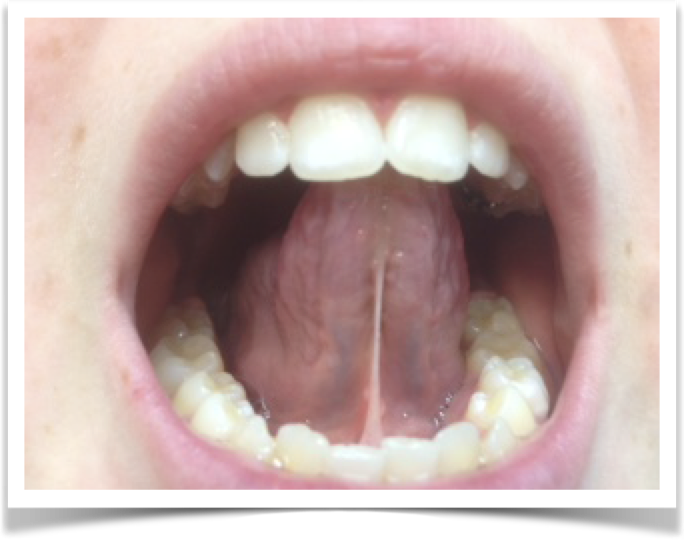
There are various options, both surgical and non-surgical, for treating tongue-tie and lip-tie. One traditional option is in-office procedure known as a frenectomy (alternatively, frenulectomy, frenotomy), which involves the careful “release” of the excess connective tissue to improve the range of movement of the tongue or lip(s).
The frenectomy procedure can be performed with either a simple surgical implement or a dental laser intended for the oral cavity’s soft tissue. The process itself is relatively quick, as is recovery. However, Dr. Robbins emphasizes the importance of parent education to ensure compliance with post-procedure exercises that facilitate healing and encourage proper motion. Myofunctional therapy also plays an essential role in treatment success.
Dr. Robbins also specializes in BabyLase, a non-surgical therapy for release of oral tissues, that take advantage of a laser’s ability to penetrate and “soften” tissue without cutting.
We encourage parents and guardians to discuss any observations or concerns they may have regarding their children’s sleep habits and any signs that may suggest sleep and breathing issues.
